Handbook Of Emergency Cardiovascular Care For Healthcare Providers Pdf Free Download
Pulmonary edema is astute, severe left ventricular failure with pulmonary venous hypertension and alveolar flooding. Findings are severe dyspnea, diaphoresis, wheezing, and sometimes blood-tinged frothy sputum. Diagnosis is clinical and past chest 10-ray. Treatment is with oxygen, Four nitrates, diuretics, and sometimes morphine and, in patients with eye failure and reduced ejection fraction short-term IV positive inotropes , and assisted ventilation (ie, endotracheal intubation with mechanical ventilation or bilevel positive airway force per unit area ventilation).
If left ventricular (LV) filling pressure increases suddenly, plasma fluid moves rapidly from pulmonary capillaries into interstitial spaces and alveoli, causing pulmonary edema. Although precipitating causes vary by age and country, nigh ane one-half of cases outcome from astute coronary ischemia Overview of Coronary Artery Disease Coronary artery illness (CAD) involves impairment of blood flow through the coronary arteries, nearly commonly by atheromas. Clinical presentations include silent ischemia, angina pectoris, astute... read more 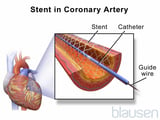 ; some from decompensation of significant underlying heart failure Heart Failure (HF) Heart failure (HF) is a syndrome of ventricular dysfunction. Left ventricular failure causes shortness of breath and fatigue, and right ventricular failure causes peripheral and abdominal fluid... read more
; some from decompensation of significant underlying heart failure Heart Failure (HF) Heart failure (HF) is a syndrome of ventricular dysfunction. Left ventricular failure causes shortness of breath and fatigue, and right ventricular failure causes peripheral and abdominal fluid... read more  (HF), including HF with preserved ejection fraction Heart failure with preserved ejection fraction (HFpEF) Center failure (HF) is a syndrome of ventricular dysfunction. Left ventricular failure causes shortness of jiff and fatigue, and right ventricular failure causes peripheral and abdominal fluid... read more
(HF), including HF with preserved ejection fraction Heart failure with preserved ejection fraction (HFpEF) Center failure (HF) is a syndrome of ventricular dysfunction. Left ventricular failure causes shortness of jiff and fatigue, and right ventricular failure causes peripheral and abdominal fluid... read more  (HFpEF) due to hypertension Hypertension Hypertension is sustained elevation of resting systolic blood force per unit area (≥ 130 mm Hg), diastolic blood pressure (≥ 80 mm Hg), or both. Hypertension with no known cause (chief; formerly, essential... read more
(HFpEF) due to hypertension Hypertension Hypertension is sustained elevation of resting systolic blood force per unit area (≥ 130 mm Hg), diastolic blood pressure (≥ 80 mm Hg), or both. Hypertension with no known cause (chief; formerly, essential... read more  ; and the rest from arrhythmia Overview of Arrhythmias The normal middle beats in a regular, coordinated manner because electrical impulses generated and spread by myocytes with unique electrical properties trigger a sequence of organized myocardial... read more
; and the rest from arrhythmia Overview of Arrhythmias The normal middle beats in a regular, coordinated manner because electrical impulses generated and spread by myocytes with unique electrical properties trigger a sequence of organized myocardial... read more 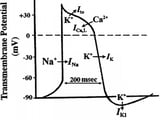 , an acute valvular disorder Overview of Cardiac Valvular Disorders Any heart valve can go stenotic or insufficient (also termed regurgitant or incompetent), causing hemodynamic changes long before symptoms. Virtually oftentimes, valvular stenosis or insufficiency... read more than , or acute book overload often due to Four fluids. Drug or dietary nonadherence is often involved.
, an acute valvular disorder Overview of Cardiac Valvular Disorders Any heart valve can go stenotic or insufficient (also termed regurgitant or incompetent), causing hemodynamic changes long before symptoms. Virtually oftentimes, valvular stenosis or insufficiency... read more than , or acute book overload often due to Four fluids. Drug or dietary nonadherence is often involved.
Symptoms and Signs of Pulmonary Edema
Patients present with farthermost dyspnea, restlessness, and anxiety with a sense of suffocation. Coughing producing blood-tinged sputum, pallor, cyanosis, and marked diaphoresis are mutual; some patients froth at the rima oris. Frank hemoptysis is uncommon. The pulse is rapid and depression volume, and blood force per unit area (BP) is variable. Marked hypertension indicates significant cardiac reserve; hypotension with systolic BP < 100 mg Hg is ominous. Inspiratory fine crackles are widely dispersed anteriorly and posteriorly over both lung fields. Marked wheezing (cardiac asthma) may occur. Noisy respiratory efforts oft make cardiac auscultation difficult; a summation gallop—merger of third (S3) and quaternary (S4) heart sounds—may exist present. Signs of right ventricular (RV) failure (eg, neck vein distention, peripheral edema) may be present.
-
Clinical evaluation showing astringent dyspnea and pulmonary crackles
-
Chest ten-ray
-
Sometimes serum encephalon natriuretic peptide (BNP) or Northward-terminal-pro BNP (NT-pro-BNP)
-
ECG, cardiac markers, and other tests for etiology as needed
A chest x-ray, done immediately, is usually diagnostic, showing marked interstitial edema. Bedside measurement of serum BNP/NT-proBNP levels (elevated in pulmonary edema; normal in COPD exacerbation) is helpful if the diagnosis is in doubt.
ECG, pulse oximetry, and blood tests (cardiac markers, electrolytes, BUN [claret urea nitrogen], creatinine and, for severely ill patients, arterial blood gas [ABG] measurements) are done.
Echocardiography may be helpful to determine the crusade of the pulmonary edema (eg, myocardial infarction Astute Myocardial Infarction (MI) Acute myocardial infarction is myocardial necrosis resulting from acute obstacle of a coronary artery. Symptoms include chest discomfort with or without dyspnea, nausea, and diaphoresis.... read more  , valvular dysfunction Overview of Cardiac Valvular Disorders Any heart valve can become stenotic or insufficient (also termed regurgitant or incompetent), causing hemodynamic changes long earlier symptoms. Almost often, valvular stenosis or insufficiency... read more , hypertensive heart illness Hypertension Hypertension is sustained elevation of resting systolic claret pressure (≥ 130 mm Hg), diastolic blood pressure (≥ 80 mm Hg), or both. Hypertension with no known crusade (primary; formerly, essential... read more
, valvular dysfunction Overview of Cardiac Valvular Disorders Any heart valve can become stenotic or insufficient (also termed regurgitant or incompetent), causing hemodynamic changes long earlier symptoms. Almost often, valvular stenosis or insufficiency... read more , hypertensive heart illness Hypertension Hypertension is sustained elevation of resting systolic claret pressure (≥ 130 mm Hg), diastolic blood pressure (≥ 80 mm Hg), or both. Hypertension with no known crusade (primary; formerly, essential... read more 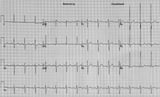 , dilated cardiomyopathy Dilated Cardiomyopathy Dilated cardiomyopathy is myocardial dysfunction causing heart failure in which ventricular dilation and systolic dysfunction predominate. Symptoms include dyspnea, fatigue, and peripheral edema... read more than
, dilated cardiomyopathy Dilated Cardiomyopathy Dilated cardiomyopathy is myocardial dysfunction causing heart failure in which ventricular dilation and systolic dysfunction predominate. Symptoms include dyspnea, fatigue, and peripheral edema... read more than  ) and may influence the choice of therapies.
) and may influence the choice of therapies.
Hypoxemia can be astringent. Carbon dioxide retention is a late, ominous sign of secondary hypoventilation.
-
Treatment of cause
-
Oxygen
-
IV diuretic
-
Nitrates
-
IV inotropes
-
Morphine
-
Ventilatory assistance
Specific boosted treatment depends on etiology:
-
For astute myocardial infarction or some other acute coronary syndrome, thrombolysis or directly percutaneous coronary angioplasty with or without stent placement
-
For severe hypertension, an Iv vasodilator
-
For supraventricular or ventricular tachycardia, direct-current cardioversion
-
For rapid atrial fibrillation, cardioversion is preferred. To tiresome the ventricular rate, an 4 beta-blocker, IV digoxin, or cautious use of an Four calcium aqueduct blocker
In patients with astute MI, fluid status earlier onset of pulmonary edema is usually normal, and then diuretics are less useful than in patients with acute decompensation of chronic heart failure and may precipitate hypotension. If systolic BP falls < 100 mm Hg or shock develops, IV dobutamine and an intra-aortic balloon pump (counterpulsation) may be required.
Some newer drugs, such as IV BNP (nesiritide), and calcium-sensitizing inotropic drugs (levosimendan, pimobendan), vesnarinone, and ibopamine, may have initial beneficial effects but do not appear to meliorate outcomes compared to standard therapy, and mortality may exist increased. Serelaxin, a recombinant form of the human being pregnancy hormone relaxin-two, has been tried merely benefits were non shown in a large international randomized study. Omecamtiv mecarbil, an oral cardiac myosin activator, is being evaluated for ability to reduce morbidity and bloodshed in patients currently or recently hospitalized with decompensated heart failure.
-
Astute pulmonary edema can issue from acute coronary ischemia, decompensation of underlying middle failure, arrhythmia, an acute valvular disorder, or acute volume overload.
-
Patients accept severe dyspnea, diaphoresis, wheezing, and sometimes blood-tinged frothy sputum.
-
Clinical examination and chest x-ray are ordinarily sufficient for diagnosis; ECG, cardiac markers, and sometimes echocardiography are washed to identify cause.
-
Treat the cause and give oxygen and Four furosemide and/or nitrates as needed; endeavor noninvasive ventilatory assistance initially only use tracheal intubation and assisted ventilation if necessary.

© 2022 Merck Abrupt & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA
DOWNLOAD HERE
Posted by: patriciafeby1967.blogspot.com